
Breast Procedures
Breast Augmentation
10 Harley Street
London W1G 9PF
Breast Augmentation
Aim: Increase the breast size with mammary prostheses.
Have you always had small breasts and perceive it as a problem?
It might be the right time to address the problem and finally find the solution to it
once and for all.
WHAT KIND OF RESULTS YOU WOULD LIKE TO ACHIEVE FROM YOUR BREAST AUGMENTATION PROCEDURE
NATURAL – A result that resembles as much as possible real breasts and that is in perfect proportion with the rest of the body. Looking at it should give you the impression that you could have been borne with it.
It’s the type of result that most of my patients request and it is what I have been always advocating and wholeheartedly recommending.
FAKE – It is the kind of look that cannot really be confused with the appearance of real breasts. With some very rare exceptions, it should always be avoided because the excessively large dimensions of the implants and their excessive weight could easily lead to breast sagginess, stretch marks, rippling and other problems, in addition to causing disharmony with the rest of the body. It is a type of look characterised by an unnatural fullness of the upper pole and an extremely and over-defined round shape. There are now fewer patients requesting this type of result in London.

CHOSING YOUR IMPLANTS SHAPE
The shape of the prostheses will determine, together with the shape of the existing patient’s breast, how natural the result will be
Anatomical (so called Teardrop implants) are preferred when the patient has extremely small breasts or virtually no breasts at all, and it is necessary to give them some shape in addition to volume.
Round implants are preferred when the existing breasts already have some volume and the aim is to enhance the existing volume.
QUALITY
When deciding to undergo breast augmentation surgery, the conversation regarding implant options should only include brands that provide the best quality, guaranteed by the strictest quality check tests. Based on the universal principle that nothing if for free in this world, if the prostheses’ cost is very low, their quality is equally low.
I personally only use the following brands: Mentor, Motiva and Nagor.
MATERIAL
I only use implants that are made of cohesive silicone gel, so called “gummy bear implants”.
These are the latest generation of implants that provide the highest safety standards and that are approved by the American FDA (Food and Drug Administration).
For Breast Augmentation procedures in London, I do not use saline-filled implants and I have never used PIP implants.


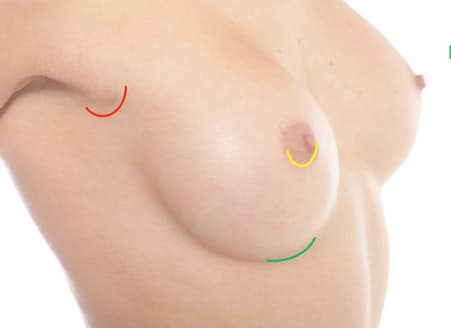
POSITION OF THE INCISION FOR BREAST AUGMENTATION
SUBMAMMARY FOLD
The submammary fold is the least traumatic and least invasive access for Breast Augmentation as we dissect under the gland tissue rather than having to cut through the gland as with the areolar approach.
In addition to allow for a quicker insertion of the prosthesis and therefore a shorter procedure, it allows for the resulting scar to be well hidden in the natural skin fold of the inframammary crease.
AREOLA
It was the access most frequently used in the past and it requires an incision placed along the inferior half circumference of the areola.
It is not always possible to utilize this access, especially when the patient has areolas with small diameter (below 3 cm).
The areolar approach has the additional disadvantage of requiring to transect, that is cut through, the entire breast gland in order to insert the implant.
Apart from rare circumstances where the surgeon has the necessity to cut through the gland and “open up” the gland in order to stretch the tissue, as for instance in the case of tuberous breasts, it would be advisable to avoid damaging the breast gland, especially in young patients.
AXILLA
The armpit is the least direct and most complex way of inserting implants; it carries disadvantages for both the surgeon and the patient.
The scar could actually end up being noticeable as women often wear sleeveless tops.
This technique is associated with a higher risk of complications such as post-opeative bleeding (haematoma), implant malpositioning and lymphedema of the breast and arm.
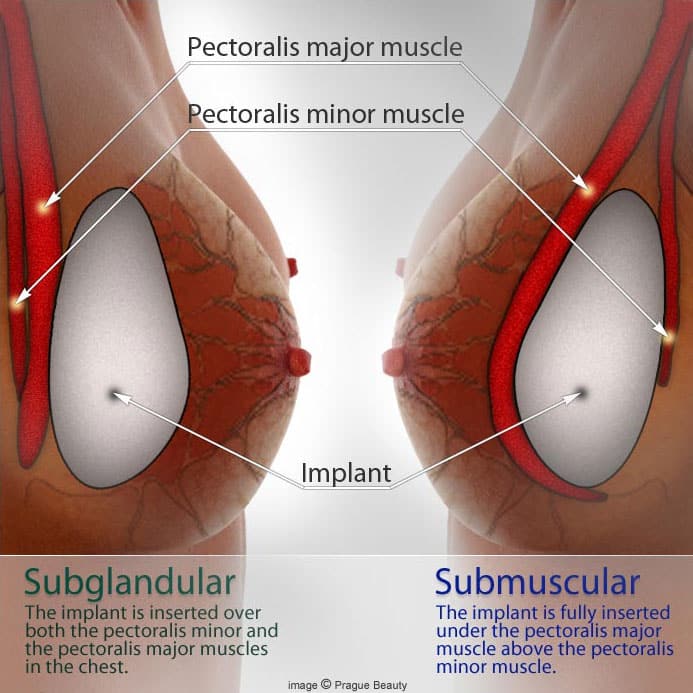
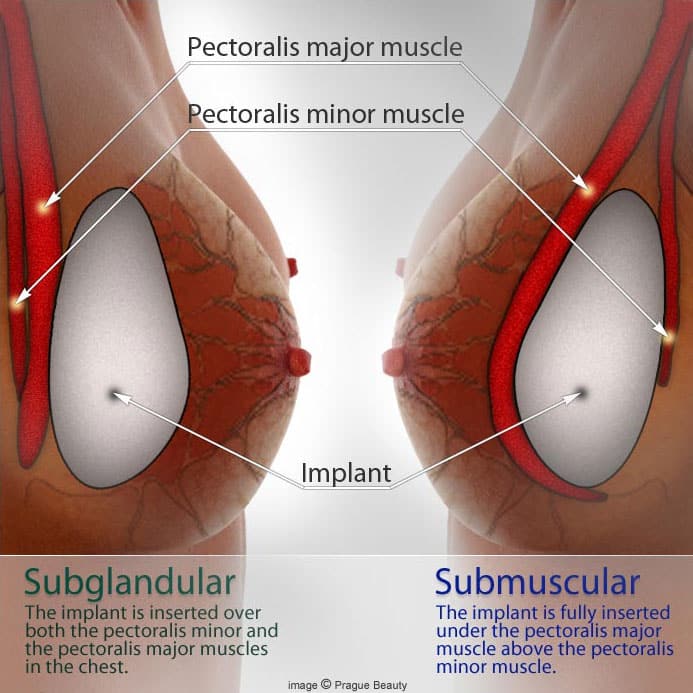
POSITION OF THE IMPLANT FOR BREAST AUGMENTATION
SUBPECTORAL DUAL PLANE
It is the most frequently used technique in thin patients with small breasts. The implant is inserted partially under the pectoralis major muscle that will cover only the upper half or upper two thirds of the implant, in order to reduce the visibility of the edges of the implant in the décolletage area.
The lower third of the implant remains subglandular in order to achieve optimal roundness and fullness in this area and a well-defined submammary fold.
SUBGLANDULAR
The prosthesis is inserted underneath the mammary gland tissue. In this case the pectoralis muscle is not utilized at all and remains as a base on top of which the implant will rest.
It is indicated for patients who perform sports activities at a professional/olympic level.
This technique allows to achieve optimal results whenever the thickness of the patient’s soft tissues (gland tissue and subcutaneous tissue) allows adequate coverage of the implant (that is, patients with at least a B cup), and when the selected implants aren’t too large.
SUBMUSCULAR
The implant is entirely covered by the pectoralis major muscle. This is a progressively less used technique for it’s results tend to appear less natural, with almost no mobility of the implants on the chest and an unnatural flattening of the lower pole of the breast.
THE SURGICAL PROCEDURE
ANEASTHESIA The surgical procedure is carried out under general anaesthesia, that is, the patient is completely asleep and fully unconscious. Normally, full intubation is not necessary and a laryngeal mask is sufficient.
Thanks to modern anaesthetic techniques, for this kind of procedure, only light anaeshtetic drug are used, in order to allow patients to wake up quickly and without severe side effects such as nausea and stupefaction.
HOSPITAL STAY
The surgical procedure is carried out in a Private Hospital as a day-case, and the patient will be admitted to a Private-Single room with en-suite bathroom, TV and Wifi connection.
The patient is admitted in the morning, and once the admission process is completed (height, weight, blood pressure, heart rate, body temperature are recorded by a nurse), the patient meets with the surgeon in order to confirm the surgical plan and sign the consent forms. The surgeon will also take pre-operative pictures of the patient and carry out surgical markings on the patient’s chest.
The patient is then taken to the operating theatre – where she is put to sleep. The surgical procedure normally takes 60-90 minutes. After a brief stay in the recovery room, where the patient is closely monitored, she will then be taken back, perfectly awake, to her room. During the course of the day the patient will be assisted with the most appropriate pain-killers and will have the opportunity to comfortably rest until the time of discharge in the afternoon.
HOSPITAL DISCHARGE
In the afternoon, once the general conditions of the patient and her ability to stand and move have been checked, the cannula (small plastic needle inserted on the back of the hand) is removed.
The patient will be able to finally look at herself fully in the mirror and have a glimpse at her breast results, prior to fitting the post-surgical bra, that she will need to wear day and night, until the first wound check.
The patient will also be provided upon discharge with the medications (antibiotics, painkillers, muscle-relaxants) for the entire week, along with the implant documents, and discharge letter.
In addition, the patient will be provided with a private telephone number active 24 hours a day that will enable her to contact the Nurse if needed (emergency number).

AFTER SURGERY
RECOVERY FROM BREAST AUGMENTATION
The vast majority of patients experiences most discomfort during the first 3 days. Pain threshold varies widely among patients. The variable amount of pain experienced is however always manageable thanks to the strong painkiller medication provided upon discharge.
During these first few days patients should be resting in bed or on a comfortable sofa, with chest elevated at a 45 degree angle.
After 10 days, most patients will go back to work.
It is advisable to avoid full showers or full baths for 4 weeks in order to allow the wounds to heal. During this time, patients should resort to sink washing, wet soaped flannels, wet wipes.
No driving, no house-work, no lifting is allowed for the first 2 weeks.
Sports activities can be resumed after 2 – 3 months.
CHECKUPS AFTER BREAST AUGMENTATION
The first wound check takes place approximately 10 days after the surgery.
Dressings are removed, wounds are inspected/checked and cleaned; new dressings are finally applied.
The second wound check takes place 14 days after the first.
At this stage normally the dressings are replaced with tiny plasters (steri-strips) and patients are authorized to have quick full showers .
The wounds take approximately 14 – 21 days to fully heal and it is crucial for the area to be kept perfectly dry during the first 4 weeks.
The stitches used are all dissolvable sutures, which don’t require being taken out or trimming.
Dr Fiumara reviews her patients 1 month, 4 months and 12 months after the surgery.
POSSIBLE RISKS AND COMPLICATIONS
When patients carefully follow the post-operative guidance provided by the surgical Team, complications are fortunately an extremely rare event.
Complications that occur within the first 24-72 hours are most often caused by internal bleeding which can lead to a haematoma (collection of blood in the surgical pocket-cavity where the implant is lodged/located).
Small haematomas can be reabsorbed spontaneously by the body.
A large haematoma instead has to be evacuated/drained in surgery.
Complications which occur at a later stage include implant dislocation and capsular contracture (excessive buildup of scar tissue around one of the implants, caused by an abnormal individual reaction of the body towards one of the implants).
During the surgical consultation, the surgeon will inform the patient about the most common risks and complications linked to the surgery and will also discuss the possible solutions.
The consent forms provided at the end of the consultation, and that the patient will have to sign on the day of the surgery, also explain in further detail the possible risks and complications of surgery.

FAQ
Q. When should implants be positioned behind the muscle and when should they be positioned in front of the muscle?
A. The decision as to whether implants should be positioned in front or behind the muscle is based on several criteria:
- Quantity of soft-tissue-coverage available to hide an implant:
Patients that have a sufficient amount of breast tissue to begin with (eg. B/C cup) can opt for implants being inserted on top of the muscle.
On the contrary, patients with very small breasts (A/AA cup) will have their implants preferably positioned behind the muscle for better coverage (in order for the implants not to show through the skin).
- Quality of the skin envelope:
Patients with extremely good quality of their breasts’ skin envelope (tight/thick/young skin) are suitable candidates for implants in front of the muscle.
On the contrary, patients with poor quality skin envelope (soft, thin, stretchy, mature/ageing skin) are better suited for subpectoral implants, in order to avoid sagginess of the breasts with time.
3. Degree of engagement in sports activities:
Professional sports-women might prefer to have their implants positioned in front of their muscle in order not to reduce their physical performance and in order to avoid the temporary upward movement of the implants whenever contracting the chestwall muscles (so called “animation deformity”)
SUBPECTORAL IMPLANTS
Advantages
– Better coverage of the implants
– Less visibility, palpability and rippling of the implants
– More natural look and feel
– Subtle/natural cleavage
– More support for the implants over time
– Lower risk of breasts sagging over time
Disadvantages
– More traumatic operation
– More painful and longer recovery time
– Animation Deformity (temporary upward movement of implants when contracting the Pectoral muscles)
SUBGLANDULAR IMPLANTS
Advantages
– Less traumatic operation
– Painless and quicker recovery
– More movement of the implants on the chestwall
Disadvantages
– Less implant coverage
– Higher risk of visibility, palpability and rippling of the implants through the skin
– Higher risk of the implants sagging over time
To book a consultation call 07943 277 215 or email clinic@lindafiumara.com
Breast Procedures
Breast Augmentation
Breast Augmentation
Aim: Increase the breast size with mammary prostheses.
Have you always had small breasts and perceive it as a problem?
It might be the right time to address the problem and finally find the solution to it
once and for all.

WHAT KIND OF RESULTS YOU WOULD LIKE TO ACHIEVE FROM YOUR BREAST AUGMENTATION PROCEDURE
NATURAL – A result that resembles as much as possible real breasts and that is in perfect proportion with the rest of the body. Looking at it should give you the impression that you could have been borne with it.
It’s the type of result that most of my patients request and it is what I have been always advocating and wholeheartedly recommending.
FAKE – It is the kind of look that cannot really be confused with the appearance of real breasts. With some very rare exceptions, it should always be avoided because the excessively large dimensions of the implants and their excessive weight could easily lead to breast sagginess, stretch marks, rippling and other problems, in addition to causing disharmony with the rest of the body. It is a type of look characterised by an unnatural fullness of the upper pole and an extremely and over-defined round shape. There are now fewer patients requesting this type of result in London.

CHOSING YOUR IMPLANTS SHAPE
The shape of the prostheses will determine, together with the shape of the existing patient’s breast, how natural the result will be
Anatomical (so called Teardrop implants) are preferred when the patient has extremely small breasts or virtually no breasts at all, and it is necessary to give them some shape in addition to volume.
Round implants are preferred when the existing breasts already have some volume and the aim is to enhance the existing volume.
QUALITY
When deciding to undergo breast augmentation surgery, the conversation regarding implant options should only include brands that provide the best quality, guaranteed by the strictest quality check tests. Based on the universal principle that nothing if for free in this world, if the prostheses’ cost is very low, their quality is equally low.
I personally only use the following brands: Mentor, Motiva and Nagor.
MATERIAL
I only use implants that are made of cohesive silicone gel, so called “gummy bear implants”.
These are the latest generation of implants that provide the highest safety standards and that are approved by the American FDA (Food and Drug Administration).
For Breast Augmentation procedures in London, I do not use saline-filled implants and I have never used PIP implants.

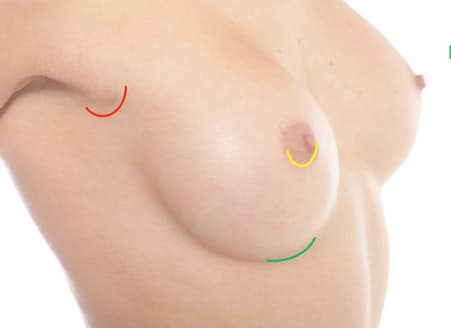
POSITION OF THE INCISION FOR BREAST AUGMENTATION
SUBMAMMARY FOLD
The submammary fold is the least traumatic and least invasive access for Breast Augmentation as we dissect under the gland tissue rather than having to cut through the gland as with the areolar approach.
In addition to allow for a quicker insertion of the prosthesis and therefore a shorter procedure, it allows for the resulting scar to be well hidden in the natural skin fold of the inframammary crease.
AREOLA
It was the access most frequently used in the past and it requires an incision placed along the inferior half circumference of the areola.
It is not always possible to utilize this access, especially when the patient has areolas with small diameter (below 3 cm).
The areolar approach has the additional disadvantage of requiring to transect, that is cut through, the entire breast gland in order to insert the implant.
Apart from rare circumstances where the surgeon has the necessity to cut through the gland and “open up” the gland in order to stretch the tissue, as for instance in the case of tuberous breasts, it would be advisable to avoid damaging the breast gland, especially in young patients.
AXILLA
The armpit is the least direct and most complex way of inserting implants; it carries disadvantages for both the surgeon and the patient.
The scar could actually end up being noticeable as women often wear sleeveless tops.
This technique is associated with a higher risk of complications such as post-opeative bleeding (haematoma), implant malpositioning and lymphedema of the breast and arm.
POSITION OF THE IMPLANT FOR BREAST AUGMENTATION
SUBPECTORAL DUAL PLANE
It is the most frequently used technique in thin patients with small breasts. The implant is inserted partially under the pectoralis major muscle that will cover only the upper half or upper two thirds of the implant, in order to reduce the visibility of the edges of the implant in the décolletage area.
The lower third of the implant remains subglandular in order to achieve optimal roundness and fullness in this area and a well-defined submammary fold.
SUBGLANDULAR
The prosthesis is inserted underneath the mammary gland tissue. In this case the pectoralis muscle is not utilized at all and remains as a base on top of which the implant will rest.
It is indicated for patients who perform sports activities at a professional/olympic level.
This technique allows to achieve optimal results whenever the thickness of the patient’s soft tissues (gland tissue and subcutaneous tissue) allows adequate coverage of the implant (that is, patients with at least a B cup), and when the selected implants aren’t too large.
SUBMUSCULAR
The implant is entirely covered by the pectoralis major muscle. This is a progressively less used technique for it’s results tend to appear less natural, with almost no mobility of the implants on the chest and an unnatural flattening of the lower pole of the breast.

THE SURGICAL PROCEDURE
ANEASTHESIA The surgical procedure is carried out under general anaesthesia, that is, the patient is completely asleep and fully unconscious. Normally, full intubation is not necessary and a laryngeal mask is sufficient.
Thanks to modern anaesthetic techniques, for this kind of procedure, only light anaeshtetic drug are used, in order to allow patients to wake up quickly and without severe side effects such as nausea and stupefaction.
HOSPITAL STAY
The surgical procedure is carried out in a Private Hospital as a day-case, and the patient will be admitted to a Private-Single room with en-suite bathroom, TV and Wifi connection.
The patient is admitted in the morning, and once the admission process is completed (height, weight, blood pressure, heart rate, body temperature are recorded by a nurse), the patient meets with the surgeon in order to confirm the surgical plan and sign the consent forms. The surgeon will also take pre-operative pictures of the patient and carry out surgical markings on the patient’s chest.
The patient is then taken to the operating theatre – where she is put to sleep. The surgical procedure normally takes 60-90 minutes. After a brief stay in the recovery room, where the patient is closely monitored, she will then be taken back, perfectly awake, to her room. During the course of the day the patient will be assisted with the most appropriate pain-killers and will have the opportunity to comfortably rest until the time of discharge in the afternoon.
HOSPITAL DISCHARGE
In the afternoon, once the general conditions of the patient and her ability to stand and move have been checked, the cannula (small plastic needle inserted on the back of the hand) is removed.
The patient will be able to finally look at herself fully in the mirror and have a glimpse at her breast results, prior to fitting the post-surgical bra, that she will need to wear day and night, until the first wound check.
The patient will also be provided upon discharge with the medications (antibiotics, painkillers, muscle-relaxants) for the entire week, along with the implant documents, and discharge letter.
In addition, the patient will be provided with a private telephone number active 24 hours a day that will enable her to contact the Nurse if needed (emergency number).

AFTER SURGERY
RECOVERY FROM BREAST AUGMENTATION
The vast majority of patients experiences most discomfort during the first 3 days. Pain threshold varies widely among patients. The variable amount of pain experienced is however always manageable thanks to the strong painkiller medication provided upon discharge.
During these first few days patients should be resting in bed or on a comfortable sofa, with chest elevated at a 45 degree angle.
After 10 days, most patients will go back to work.
It is advisable to avoid full showers or full baths for 4 weeks in order to allow the wounds to heal. During this time, patients should resort to sink washing, wet soaped flannels, wet wipes.
No driving, no house-work, no lifting is allowed for the first 2 weeks.
Sports activities can be resumed after 2 – 3 months.
CHECKUPS AFTER BREAST AUGMENTATION
The first wound check takes place approximately 10 days after the surgery.
Dressings are removed, wounds are inspected/checked and cleaned; new dressings are finally applied.
The second wound check takes place 14 days after the first.
At this stage normally the dressings are replaced with tiny plasters (steri-strips) and patients are authorized to have quick full showers .
The wounds take approximately 14 – 21 days to fully heal and it is crucial for the area to be kept perfectly dry during the first 4 weeks.
The stitches used are all dissolvable sutures, which don’t require being taken out or trimming.
Dr Fiumara reviews her patients 1 month, 4 months and 12 months after the surgery.
POSSIBLE RISKS AND COMPLICATIONS
When patients carefully follow the post-operative guidance provided by the surgical Team, complications are fortunately an extremely rare event.
Complications that occur within the first 24-72 hours are most often caused by internal bleeding which can lead to a haematoma (collection of blood in the surgical pocket-cavity where the implant is lodged/located).
Small haematomas can be reabsorbed spontaneously by the body.
A large haematoma instead has to be evacuated/drained in surgery.
Complications which occur at a later stage include implant dislocation and capsular contracture (excessive buildup of scar tissue around one of the implants, caused by an abnormal individual reaction of the body towards one of the implants).
During the surgical consultation, the surgeon will inform the patient about the most common risks and complications linked to the surgery and will also discuss the possible solutions.
The consent forms provided at the end of the consultation, and that the patient will have to sign on the day of the surgery, also explain in further detail the possible risks and complications of surgery.
FAQ
Q. When should implants be positioned behind the muscle and when should they be positioned in front of the muscle?
A. The decision as to whether implants should be positioned in front or behind the muscle is based on several criteria:
- Quantity of soft-tissue-coverage available to hide an implant:
Patients that have a sufficient amount of breast tissue to begin with (eg. B/C cup) can opt for implants being inserted on top of the muscle.
On the contrary, patients with very small breasts (A/AA cup) will have their implants preferably positioned behind the muscle for better coverage (in order for the implants not to show through the skin).
- Quality of the skin envelope:
Patients with extremely good quality of their breasts’ skin envelope (tight/thick/young skin) are suitable candidates for implants in front of the muscle.
On the contrary, patients with poor quality skin envelope (soft, thin, stretchy, mature/ageing skin) are better suited for subpectoral implants, in order to avoid sagginess of the breasts with time.
3. Degree of engagement in sports activities:
Professional sports-women might prefer to have their implants positioned in front of their muscle in order not to reduce their physical performance and in order to avoid the temporary upward movement of the implants whenever contracting the chestwall muscles (so called “animation deformity”)
SUBPECTORAL IMPLANTS
Advantages
– Better coverage of the implants
– Less visibility, palpability and rippling of the implants
– More natural look and feel
– Subtle/natural cleavage
– More support for the implants over time
– Lower risk of breasts sagging over time
Disadvantages
– More traumatic operation
– More painful and longer recovery time
– Animation Deformity (temporary upward movement of implants when contracting the Pectoral muscles)
SUBGLANDULAR IMPLANTS
Advantages
– Less traumatic operation
– Painless and quicker recovery
– More movement of the implants on the chestwall
Disadvantages
– Less implant coverage
– Higher risk of visibility, palpability and rippling of the implants through the skin
– Higher risk of the implants sagging over time
As featured in The Evening Standard and The Telegraph –








Copyright © 2023 Dr Linda Fiumara MD
Designed by Createch
